By Jerry Omondi –

The World Health Organization (WHO) is hopeful that the health emergencies that have troubled the world in 2022 will be declared over at different stages of 2023.
Speaking on Wednesday at the organization’s press briefing, Director-General Dr Tedros Adhanom pointed out that 2022 has been a challenging year , with the spread of diseases such as COVID-19, Mpox, Ebola and Cholera, in addition to other emergencies like floods and conflicts.
“We are hopeful that each of these emergencies will be declared over at different points next year,” DR Tedros said.
The WHO chief said since the peak at the end of January, the number of weekly reported COVID-19 deaths has dropped almost 90 percent.
He also noted that the number of weekly reported cases of Mpox has declined more than 90 percent from the peak.
Regarding cholera, he said vaccination programs rolled out had raised hope that the disease would be eradicated too.
Dr Tedros however asserted that there is still much to be done for the world to eradicate the health crises that have dogged it through the year.
He acknowledged, for instance, uncertainties and gaps that remain in the fight against COVID-19.
These include; gaps in surveillance, testing and sequencing; gaps in vaccination; gaps in treatment; and gaps in health systems.
20 suspected cholera deaths recorded in southern Nigeria
By Jerry Omondi
20 people are suspected to have died of cholera in southern Nigeria’s Cross River state, local Premium Times reports.
Some ten villages have been affected this week, prompting health authorities to bolster surveillance in the region.
The Permanent Secretary at the Cross River Ministry of Health, Iwara Iwara, confirmed the cholera outbreak, but did not issue an official number of resulting deaths.
A village head however said up to 20 peopla may have died of the deadly disease.
“As at Saturday, more than 20 persons have died because of suspected cholera across the 10 villages,” Premium Times quotes the unnamed village head.
Iwara gave assurances that the state government had activated a rapid health response team to tackle the outbreak.
Nigeria has been troubled by cholera outbreaks this year, some attributed to resultant floods in part sof the country following heavy rainfall.
According to reports, Borno State recorded some 5,000 cases with 178 associated deaths across 13 local government areas.
Egypt detects fourth case of moneybox
Ahram Online , Monday 12 Dec 2022
The Ministry of Health and Population announced on Monday that it had detected the country’s fourth positive case of monkeypox (Mpox) in a person who was in contact with the previously infected individual. Monkeypox
According to the ministry, the 34-year-old patient’s condition is stable and he is currently being treated at one of the ministry’s hospitals.
The patient was in close contact with one of the previously detected cases, a 39-year-old who resides in a European country on a visit to Egypt, which was announced on 8 December.
Egypt officially detected its first monkeypox case in early September.
The Mpox virus was first discovered in 1958.
According to the World Health Organisation (WHO), Mpox primarily occurs in central and west Africa, often in proximity to tropical rainforests, but has been increasingly appearing in urban areas.
As a viral zoonotic infection, it can spread from animals to humans and can also spread from person to person through close contact, including sexual contact.
Several Arab countries reported cases of Mpox in the past months, including UAE, Lebanon, Bahrain, Saudi Arabia and Morocco
Africa Continues to Shoulder Heaviest Malaria Burden – WHO Report

By Melody Chironda
Each year, the World Health Organization, WHO’s World malaria report provides a comprehensive and up-to-date assessment of trends in malaria control and elimination across the globe.
Malaria is a life-threatening disease caused by parasites that are transmitted to people through the bites of infected female Anopheles mosquitoes. Symptoms, including fever, headache, and chills usually appear 10-15 days after a bite and may be mild and difficult to recognize as malaria. Left untreated, malaria can progress to severe illness and death. It is preventable and curable.
WHO has released new data that shows that countries around the world largely held the line against further setbacks to malaria prevention, testing, and treatment services in 2021. According to WHO’s latest report, there were an estimated 619,000 malaria deaths globally in 2021 compared to 625,000 in the first year of the pandemic. In 2019, before the pandemic struck, the number of deaths stood at 568,000.
In 2020, there were an estimated 241 million cases of malaria worldwide and the estimated number of malaria deaths stood at 627,000 in 2020. In the past two decades, the annual death rate from malaria has dropped by nearly half, making it one of humanity’s greatest public health successes.
The African region continues to shoulder the heaviest burden of malaria. In 2021, the region accounted for 95% of all malaria cases (234 million cases) and 96% of all malaria deaths (593 000 deaths). Children under 5 years of age accounted for about 80% of all malaria deaths.
Four countries also accounted for just over half of all malaria deaths globally: Nigeria (31.3%), the Democratic Republic of the Congo (12.6%), the United Republic of Tanzania (4.1%), and Niger (3.9%). Nigeria accounted for an estimated 38.4% of global malaria deaths in children aged under 5 years. Malaria remains a primary cause of childhood illness and death in sub-Saharan Africa. Africa is struggling to eliminate the disease.
Progress varied, however, and some individual countries beat the overall regional trend. Between 2015 and 2021, Cabo Verde, Ethiopia, the Gambia, Ghana, Mauritania, Rwanda, South Africa, and Zimbabwe met the target of a reduction in malaria case incidence of 40% or more.
Although not on track to reach the GTS milestones, 15 countries achieved reductions in malaria case incidence, Burkina Faso, Cameroon, Equatorial Guinea, Eswatini, Guinea, Kenya, Malawi, Mali, Mozambique, Niger, Senegal, Sierra Leone, Togo, Tanzania, and Zambia. Cabo Verde and Eswatini had zero estimated malaria deaths in 2021, while Ethiopia, South Africa, and Zimbabwe achieved reductions in their mortality rates of 40% or more. Algeria was certified malaria-free by WHO in 2019.
Matshidiso Moeti, WHO Regional Director for Africa, said “despite progress, the African region continues to be hardest hit by this deadly disease … new tools – and the funding to deploy these – are urgently needed to help us defeat malaria”.
Disruptions during the pandemic and converging humanitarian crises, health system challenges, restricted funding, rising biological threats and a decline in the effectiveness of core disease-cutting tools threaten the global response to malaria, the report added.
The report also found that malaria progress is being hampered by the declining effectiveness of core malaria control tools, such as ITNs. Threats to this key prevention tool include insecticide resistance; insufficient access; loss of ITNs due to the stresses of day-to-day use outpacing replacement; and changing behaviour of mosquitoes, which appear to be biting early before people go to bed and resting outdoors, thereby evading exposure to insecticides.
Other risks are also rising, including parasite mutations affecting the performance of rapid diagnostic tests; growing parasite resistance to the drugs used to treat malaria, and the invasion in Africa of an urban-adapted mosquito that is resistant to many of the insecticides used today.
The latest World Malaria Report shows that U.S.$7.3 billion is required globally to stay on track to defeat malaria.
WHO recently launched two strategies to support countries in the African continent as they work to build a more resilient response to malaria: a strategy to curb antimalarial drug resistance and an initiative to stop the spread of the Anopheles stephensi malaria vector. Additionally, a new global framework to respond to malaria in urban areas, developed jointly by WHO and UN-Habitat, provides guidance for city leaders and malaria stakeholders.
Malawi and WHO recently rolled out a new malaria vaccine for young children that backers say will reduce deaths from the mosquito-borne disease. Malawi begun vaccinating children as part of a world-first, large-scale campaign against malaria using the RTS,S vaccine which was tested in Ghana, Kenya, and Malawi. It has taken more than 30 years to develop the vaccine. Malaria remains a huge public health problem in Malawi, with about one-third of its 20 million people getting infected each year. In 2021, the government launched a nationwide anti-malaria initiative known as Zero Malaria Starts with Me, aimed at eliminating the disease by 2030.
In August 2022, Nigeria’s President Buhari inaugurated the 16-member committee, which will oversee an effort to eliminate malaria in Nigeria within the next eight years. He appointed Aliko Dangote, Africa’s richest man, to lead a committee commissioned with eliminating malaria in the West African nation as the mosquito-borne infection has made a comeback across the continent amid disruptions related to the coronavirus pandemic. The World Health Organization says Nigeria alone accounts for about 27% of all malaria cases and 31.3% of malaria deaths globally.
Africa CDC convenes public health officials and experts to prepare the continent to respond to future outbreaks

Public health officials, experts, researchers, and scientists around Africa will gather at a major conference at the African Union Commission in Addis Ababa, Ethiopia, this week to take stock of how ready, in a post-COVID-19 world, African countries are to face up to the next disease threat.
‘Beyond COVID-19: Pathogen Genomics and Bioinformatics for Health Security in Africa’ will be hosted by the Africa Centres for Disease Control and Prevention (Africa CDC), the autonomous health institution of the African Union (AU). The meeting will be held at the AU’s Headquarters in Addis Ababa from 29 November to 1 December 2022.
The event will draw around 120 public health officials, researchers, and scientists from 49 AU Member States, as well as local and international partners.
The symposium will, in particular, focus on the existing capacity along the full value chain of pathogen genomics and bioinformatics. This entails everything from the sequencing and analysing of disease-causing pathogens, to issues of supply chain, the generation and sharing of data, as well as international policies and agreements that govern how these processes should unfold.
Participants will review the progress, challenges and lessons from the rapid expansion of pathogen genomics in Africa, through the Africa CDC’s Africa Pathogen Genomics Initiative (Africa PGI) and the work of other stakeholders over the past two years.
These endeavours all form part of the mission of the Africa CDC, which was launched in 2017, to coordinate continent-wide responses to emerging, re-emerging and other diseases in African countries, explains Dr Sofonias Tessema, programme lead for pathogen genomics at Africa CDC. The capacity in pathogen genomics, which is key to effective emergency response, was sorely lacking, he notes.
“Africa bears a disproportionate disease burden, and we face many deadly outbreaks every year, from Ebola and Cholera to Yellow Fever and polio,” says Dr Tessema. “Therefore, one of the foundational flagship projects of Africa CDC has been the setting up of capacity for pathogen sequencing around the continent. The project was initiated well before emergence of COVID-19, but it has certainly gained momentum because of the pandemic.”
“COVID-19 is a painful reminder of how ill prepared the continent was,” points out Dr Yenew Kebede, Head of the Division of Laboratory Systems and Network and Acting Head of Division of Surveillance and Disease Intelligence at Africa CDC.
In 2019, only seven of the 55 African Union Member States had public health laboratories or affiliates with next-generation sequencing (NGS) capacity. When COVID-19 hit the world in 2020, Africa CDC – working closely with the World Health Organisation’s Africa Regional Office (WHO AFRO) and other partners – was very quickly able to roll out sequencing technologies and training as countries and international agencies struggled to monitor the pandemic and keep track of emerging variants of SARS-CoV-2, the coronavirus causing the COVID-19 disease.
Today, public health laboratories in at least 37 African countries have NGS capacity, with training and equipment planned to be rolled out to even more African countries.
“No one would have asked for a global pandemic with its tragic human, social and economic costs,” says Dr Kebede. “But in exposing our shortcomings, COVID-19 also allowed us to do within a year or two what may have taken much longer under different circumstances.”
Efforts are now also under way to build on that momentum.
“We are now ready for the next phase, as the Africa PGI moves beyond COVID-19 and as attention shifts back to more local and regional disease outbreaks,” says Prof Alan Christoffels, Director of the South African National Bioinformatics Institute (SANBI) at the University of the Western Cape in South Africa, and Senior Advisor to Africa CDC. “It has now become more urgent that we capacitate individual countries.
SANBI is one of three specialist genomics and bioinformatics centres that initially served as the backbone of Africa CDC’s genomic sequencing programme, lending support to nine regional hubs around the continent.”
These hubs are public health laboratories able to sequence SARS-CoV-2 pathogens, services that each extended to its neighbouring countries.
“We are keen that all countries in Africa develop the capacity for sequencing pathogens themselves, so that they know what they are dealing with during each outbreak,” says Dr Ahmed Ogwell Ouma, Acting Director of Africa CDC. “We therefore must support individual countries to have the technology, the skills and the protocols in place to do so, as this new tool informs their response to outbreaks,
epidemics and even pandemics.”
The Addis Ababa meeting, he adds, is a critical part of ongoing work to realise this vision.
African continent finally to receive 1st mpox vaccines
AP
Africa’s top public health body says the continent is set to receive its first batch of mpox vaccines as a donation from South Korea.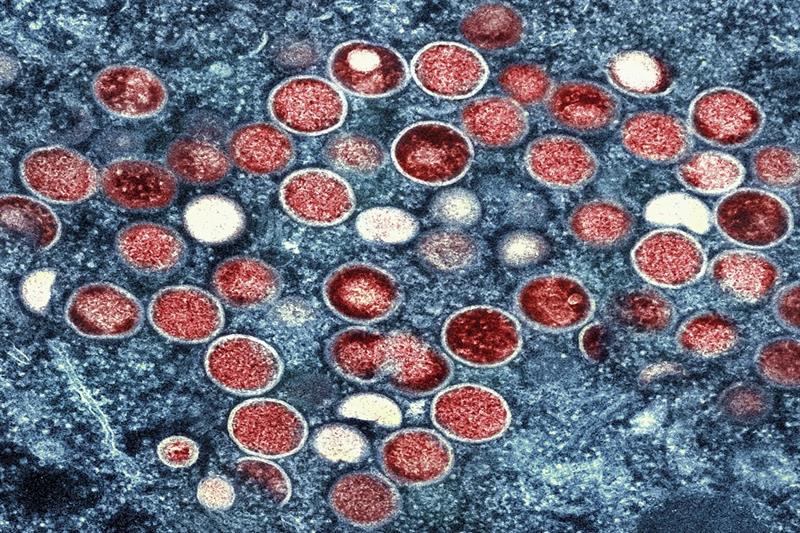
File Photo: A colorized transmission electron micrograph of monkeypox particles (red) found within an infected cell (blue), cultured in the laboratory that was captured and color-enhanced at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Md. AP
The Africa Centers for Disease Control and Prevention said Thursday the 50,000 doses will be used first for health workers and people living in the hardest-hit areas. No timing was given for the doses’ arrival.
The continent this year has recorded 202 deaths from mpox – formerly known as mpox – with a fatality rate of 19.3% across 13 countries. And yet African health authorities for months have pursued vaccines mostly in vain as major outbreaks were reported in rich, Western countries for the first time.
Acting CDC director Ahmed Ogwell noted 51 new mpox cases in Congo in the past week and said Ghana and Nigeria are the other most affected countries.
Zimbabwe Scores Another First Against HIV In Africa
HARARE, ZIMBABWE — In October, Zimbabwe became the first African country to approve the use of the injectable HIV prevention drug called cabotegravir.
A 32-year-old Zimbabwean woman, who requested not to be identified, said she received an injection of the HIV prevention drug while she was working in the United States.
She had been taking HIV prevention pills daily for seven years. But after she received the shot in April, and now that Zimbabwe has approved it, she is hoping to take the injection every two months.
“I am excited that there is cabo in Zimbabwe,” she told VOA. “It is good news. Well, I prefer the injection to the pill because the injection is convenient. You only get a shot after every two months, unlike the pill — you have to take it every day at the same time, and there is a risk of defaulting because there are a lot of things that happen during the day. In life, actually, you might go to a funeral and forget your pills at home. With this injection, you get an injection after every two months, which is six shots per year compared to tablets.”
Zimbabwe is the first African country to approve the use of cabotegravir, or CAB-LA. The United States approved the drug in December 2021, and Australia in August 2022.
In 1999, Zimbabwe introduced a 3 percent AIDS levy to help fund the country’s response to HIV and AIDS. Individuals pay 3 percent income tax, and employers and trusts pay 3 percent on profits for the effort.
The World Health Organization has commended Zimbabwe for approving cabotegravir, saying it would pave the way to providing more safe and effective options for HIV prevention.
Farai Masekela, the head of evaluation and registration for the Medicines Control Authority of Zimbabwe, or MCAZ, says for now, cabotegravir is only allowed for HIV prevention, not treatment.
“There are going to be other preparations containing cabotegravir, which may be submitted at a later time by the applicants or manufacturers of the product which will be used for treatment,” Masekela explained. “But the current one, which was approved, is meant only for prevention of HIV, not for treatment.”
Dr. Nyaradzo Mgodi of the University of Zimbabwe Clinical Trials Research Center, who headed trials in nine African countries, said the drug is very effective and is calling for Zimbabwe to roll out cabotegravir as soon as possible.
“Because as African women, we continue getting HIV/AIDS at alarming rates, and one infection is one too many,” Mgodi said. “When we have something that works, we should make it available to the person or persons who need it.”
Supporters say access to drug will also help Zimbabweans stop relying as much on other countries for drugs to treat HIV/AIDS.
Kenya escapes international ban, World Athletics to “closely monitor” doping situation
By CGTN Africa
By Mutwiri Mutuota
Kenya, was on Wednesday, spared an international ban from athletics but the East African nation is not out of the woods yet over spiraling cases of doping.
World Athletics announced that the distance running powerhouse will continue to be monitored closely following the conclusion of its two-day Council Meeting in Rome, Italy.
World Athletics chief, Sebastian Coe cited assurances from Kenya’s government to increase funding to fight doping as the reason to spare the country from an international ban for now.

“Building trust will be a long process. We will continue to monitor Kenya closely after an assurance by the sports minister of additional funding (to anti-doping efforts),” Coe said at a press conference much to the relief of a nation that was on the brink of a ban last week.
The latest international suspension care came in the aftermath of an all-time record year for Kenyans provisionally suspended or banned for doping.
Almost 30 Kenyan runners have been banned for doping by the Athletics Independent Unit- the independent anti-doping body of World Athletics as well as the local Anti-Doping Agency of Kenya (ADAK) so far in 2022.
A further 20 or so are cases under review, a worrying state of affairs that put Kenya in the crosshairs of the world governing body with pressure mounting to ban the East African nation.

Last Friday (November 25), the newly appointed Cabinet Secretary for Sports, Heritage, and the Arts, Ababu Namwamba announced he had spoken to Coe and assured World Athletics the government increase funding for the anti-doping effort with an additional $5 million per year for the next five years.
“We laud the President of World Athletics, Lord Sebastian Coe for acknowledging our efforts in this regard.
“In his communication to me this week, Coe praised the government’s action and plan in the fight against the threat of doping,” Namwamba added in a statement.
The additional funding will go to ADAK and Athletics Kenya “to develop their testing, mobilization, reconnaissance, surveillance and enforcement capabilities.”
The Kenyan government was compelled to reach out to the world governing body amid reports its independent agency, AIU would recommend the suspension of the country from international athletics.
The AIU which, is based in the French Principality of Monaco, submitted its report on Category A countries- the nations deemed to be at the highest risk of doping- of which Kenya has been blacklisted since 2017 last Friday.
In an exclusive interview with CGTN Africa anchor, Mahia Mutua that aired in the weekly sports magazine show, Sports Scene in October, AIU chief executive, Brett Clothier had sounded a warning to drug cheats in the country that the noose was tightening around them.
“We are very, very concerned to be frank. There is far too much doping happening in Kenya in recent years.
“It’s highly concerning to us that a country that is so strong and so important to our sport has such a large doping problem. There is no getting around, that’s a fact,” Clothier remarked at the time.
He cited inadequate funding to ADAK as one of the challenges facing the anti-doping efforts in the East African nation.
“So, I think we have a reasonable platform here, we have willing partners and really good cooperation but more funding needs to be put into those domestic local authorities to assist us better in tackling the problem of doping,” the British head of the AIU advised.
Barely three weeks after the interview aired, sources within the leadership of local athletics revealed the country was on the brink of a ban, setting in motion the swift government action that has earned Kenya a stay of execution to get its house in order.
UN: Inequalities a roadblock in tackling AIDS
By Halligan Agade -36 mins ago
The United Nations has grim news about the global fight against HIV/AIDS. In a UNAIDS report released in conjunction with World AIDS day, the organisation said the world is not on track to end the AIDS pandemic because new infections are rising and AIDS deaths are continuing in too many communities.
“Inequalities are holding us back,” said Winnie Byanyima, UNAIDS Executive Director. “Simply put, the report calls the world’s attention to the painful reality that dangerous inequalities are undermining the AIDS response and jeopardizing the health security of everyone.”
The report highlights three specific areas of inequality for which concrete action must be addressed; gender inequalities, harmful masculinities, and the marginalization and criminalization of key populations, which data show is resulting in starkly little progress for those populations and undermining the overall response in addition to inequalities for children whose lives must matter more than their market share.
The report said that unequal power dynamics between men and women and harmful gender norms increase the HIV vulnerability of women and girls in all their diversity, deprive them of their voice and the ability to make decisions regarding their own lives, reduce their ability to access services that meet their needs, increase their risks of experiencing violence or other harms, and hamper their ability to mitigate the impact of AIDS.
Discrimination against and stigmatization and criminalization of some groups are costing lives and preventing the world from achieving the agreed AIDS targets. This is true in both concentrated and generalized epidemics. For example, while HIV incidence has declined since 2010 by 58 percent among adults (aged 15 to 49 years) in western and central Africa and 62 percent in eastern and southern Africa, data reveals that there was no conclusive decline among gay men and other men who have sex with men in those regions over the same period.
Furthermore, data in countries across different regions and types of epidemics such as India, Kenya, Myanmar, Nigeria and Vietnam revealed that different key populations have lower HIV service coverage compared to the general population.
Additionally, the world continues to fail children in the AIDS response. In 2021, 800 000 children living with HIV were still not on life-saving treatment. Many children are also being diagnosed late, with 60 percent of children aged 5 to 14 years living with HIV not currently receiving treatment.
The report said the inequalities aren’t merely harmful to individuals, they also impede progress against AIDS, reducing the returns on HIV investments and putting millions of people at risk. While HIV infection and AIDS are both entirely preventable, the rates of both are not declining quickly enough to put the world on course to end AIDS by 2030.
“But this is not a counsel of despair, it is a call to action. Through bold action to confront these inequalities, we can end AIDS,” adds Byanyima.
Adolescent girls and young women (aged 15 to 24 years) are three times more likely to acquire HIV than adolescent boys and young men of the same age group in sub-Saharan Africa. One study showed that enabling girls to stay in school until they complete secondary education reduces their vulnerability to HIV infection by up to 50 percent By interrupting the power dynamics, policies can reduce girls’ vulnerability to HIV. Some communities are known to deny girls education by marrying them off at a young age.
Harmful masculinities are discouraging men from seeking care. While 80 percent of women were accessing treatment in 2021, only 70 percent of men were on treatment.
Byanyima further noted that today is a moment of courage to ensure that all the girls are in school, safe and strong. To tackle gender-based violence and promote healthy masculinities and replace harmful behaviors which exacerbate risks for everyone. To decriminalize people in same-sex relationships, sex workers, and people who use drugs, and invest in community-led services that enable their inclusion to help break down barriers to services and care for millions of people.
Global statistics show that new HIV infections have reduced by 54 percent since the peak in 1996. 38.4 million were living with HIV in 2021, 1.5 million became newly infected with HIV in 2021 and 650,000 people died from AIDS-related illnesses.
Women and girls accounted for 49 percent of all new infections in 2021. Since 2010, new HIV infections have declined by 32%, from 2.2 million to 1.5 million.
In 2021, nearly 650 000 people died from AIDS-related illnesses globally compared to 2.0 million in 2004 and 1.4 million in 2010. AIDS-related mortality has declined by 57 percent among women and girls and by 47 percent among men and boys since 2010.
In sub-Saharan Africa, six in seven new HIV infections among adolescents aged 15–19 years are among girls. Girls and young women aged 15–24 years are twice as likely to be living with HIV than young men. In sub-Saharan Africa, women and girls accounted for 63 percent of all new HIV infections in 2021.
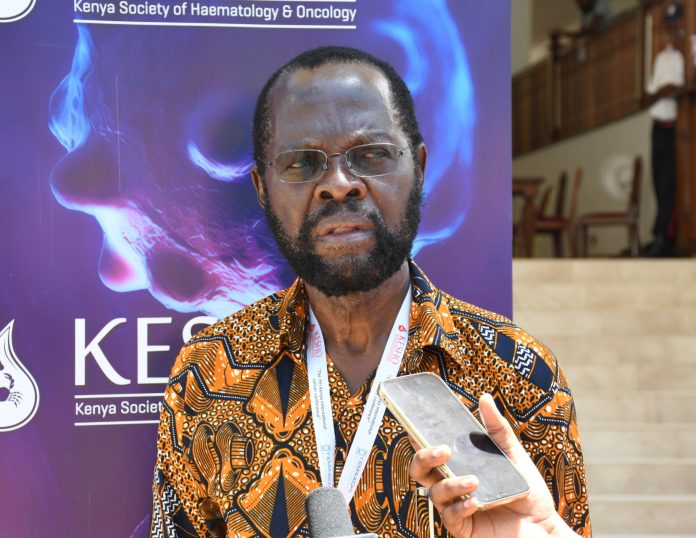
Africa urged to increase funds in fight against cancer
a cancer cell and lymphocytes
African governments must invest funding in cancer research, awareness, prevention and treatment to curb the rising numbers of cases, resulting in a massive loss of lives. This was a clarion call during the 7th Kenya International Cancer Conference that brought together haematologists, oncologists at Kenya’s seaside city of Mombasa for the three-day event from 24 to 26 November.
While addressing the conference, chairperson of the Kenya Society of Haematology and Oncology Dr. Miriam Mutebi said that the Kenyan government for instance should set aside nearly Kshs. 12 billion (0.1% of Kenya’s GDP) annually to finance targeted research on cancer, to inform the local interventions in the fight against the disease.

Additionally she submitted that research is a key pillar in matters of cancer control and of extreme significance in understanding the cancer burden and how patients respond to different treatments and interventions.
She mentioned that a lot of the cancer research being conducted in the East African country was not addressing challenges faced by Kenya.
“This is because cancer research is largely funded through external collaborators who frequently dictate the terms and areas of the research, which may not always align with the local priorities,” Dr Mutebi explained.
Dr. Gebrekrstos Hagos, a Clinical Oncologist at Needle Cancer Care Center in Hargeisa said that education on the signs and symptoms of cancer is key, coupled with increasing the capacity of health workers on early detection and referral to cancer centres.
Dr Hagos who did a study in Hargeisa said most patients admitted to oncology wards were at advanced stages of cancer, and this can be due to late presentation or long waiting time for cancer treatment.
Dr. Hagos submitted that: “The proportion of cases in developing countries will increase from 56% in 2008 to more than 60% in 2030.”
Dr. Verna Verndapuye from National Center for Radiotherapy Oncology and Nuclear Medicine Korle Bu Teaching Hospital in Accra Ghana said that adoption of Universal Health Coverage globally will help in cancer management. She added that regional cancer centers of excellence as well as increased technological skills will go along way in the fight against the disease.
On his part, Kisumu Governor Prof. Anyang Nyong’o said funding health services must be prioritized in county governments.
Prof. Nyong’o challenged medical care givers, oncology experts and supportive staff to push the agenda for increased finances to primary healthcare and preventive initiatives both at the county and national government levels.
“The cancer figures at the county level are so huge when compared to the meager resources allocated for attending to them. In fact, infrastructure and human resources are the key challenges faced by counties in their fight against cancer,” the Kisumu County Governor said. “Given the projection of cancer numbers, we should all support counties in putting in place infrastructure for cancer screening and other early detection measures.”
He also challenged stakeholders to change their approach to cancer screening to places where the targeted are. “If you are targeting men, for instance, why can’t you do such things [cancer screening] in bars and football pitches?,” he posed.
The Conference chairperson reminded delegates at the meeting that African Union member states in 2012 adopted a proposal to dedicate at least 1% of their respective GDPs for health research, adding that Kenya should move a step further by ring-fencing at least 10% of that amount for cancer research.
According to data from Globocan, the aggregate cancer burden in Africa showed 1.1 million new cases and 711,429 deaths were estimated to have occurred on the continent in 2020.
Breast cancer was the leading malignancy in females in Africa, with nearly 186,598 new cases and 85,787 deaths in 2020. Cervix uteri (cervical cancer, henceforth) was ranked second in Africa with an estimated incidence of 117,316. Prostate cancer was the leading cancer in African males with 93,173 cases and 47,249 deaths.


